Every $1 of NIH funding yields $2.46 in economic growth. A pretty good investment!
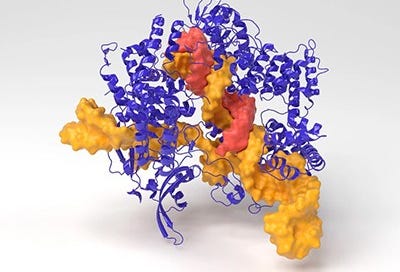
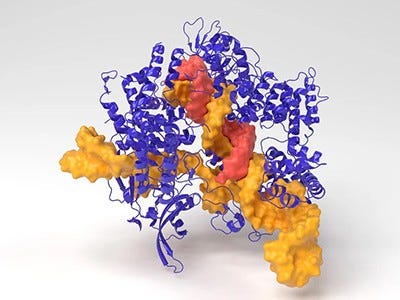
From Nature: This week scientists released the most powerful-ever AI model for biology. “The model — which was trained on 128,000 genomes spanning the tree of life, from humans to single-celled bacteria and archaea — can write whole chromosomes and small genomes from scratch. It can also make sense of existing DNA, including hard-to-interpret ‘non-coding’ gene variants that are linked to disease.
Evo-2, co-developed by researchers at the Arc Institute and Stanford University, both in Palo Alto, California, and chip maker NVIDIA, is available to scientists through web interfaces or they can download its freely available software code, data and other parameters needed to replicate the model.”
Economist Alex Tabarrok on why boosting FDA staffing would actually increase its efficiency by speeding up drug approvals. A key excerpt: “The Prescription Drug User Fee Act of 1992 (PDUFA) provides strong evidence that with more staff the FDA works faster to get new and better drugs to patients. Before PDUFA, drug approvals languished at the FDA simply due to a lack of staff—harming both drug companies and patients. Congress should have increased FDA funding, as the benefits would have far outweighed the costs, but Congress failed. Instead, PDUFA created a workaround: drug firms agreed to pay user fees, with the condition that the funds be used for drug reviewers and that the FDA be held to strict review standards…PDUFA was a tremendous success. Carpenter et al., Olson, Berndt et al. and others all find that PDUFA shortened review times and it did so primarily through the mechanism of hiring more staff. Thus, Carpenter et al. report “NDA review times shortened by 3.3 months for every 100 additional FDA staff.” Moreover, the faster approval times came at little to no expense of reduced safety.”
Some happy news, from Nature: A new cheap blood test can detect pancreatic cancer before it spreads. “Researchers have developed a simple blood test to detect pancreatic cancer before it spreads to other sites in the body. The test could be used for routine screening to improve the disease’s low survival rate1…The researchers tested the nanosensor on frozen blood samples from 356 individuals, some with pancreatic cancer, some with non-cancerous forms of pancreatic disease and healthy controls. The nanosensor correctly identified healthy individuals 98% of the time, and identified people with pancreatic cancer with 73% accuracy. It always distinguished between individuals with cancer and those with other pancreatic diseases.”
Discussion about this post
No posts


Grateful for your service curating this info! It's hard for us folks in other fields to stay up on some of public health research and news.
such good info! Thanks!